How Long To Heal A Nail Fungis W Lamisil Oral
Fungal nail infection (onychomycosis [OM]) is a mycotic infection caused by fungal invasion of the nail structure[1]
and is one of the most common nail disorders, representing one-half of nail abnormalities in adults[two]
. Its prevalence in Europe is around 4.three% over all historic period groups[3]
and 15.5% of all boom dystrophies in children[4]
. OM is more commonly diagnosed in men and older people, affecting xx–l% of people aged over 60 years[five]
. An increased incidence among older people may be attributed to multiple factors, including reduced peripheral circulation, diabetes, inactivity, relative immunosuppression, and reduced nail growth and quality[6]
. Toenails are affected more commonly than fingernails.
This commodity will cover the causes, types and handling of OM, practical information to help guide patient consultations and when to refer to podiatry.
Boom beefcake and onychomycosis infection
Figure 1 shows the composition of the smash, including the nail plate (the visible function of the nail), boom bed (the skin under the nail) and nail matrix.
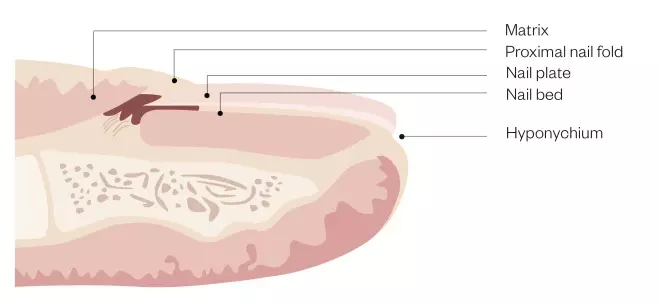
Figure 1: Smash anatomy and physiology
The smash plate and blast bed are joined past layers of hard, translucent, keratinised cells. The nail bed and nail matrix are vascular components of the nail, with nail cells located inside the nail matrix where the boom plate is formed. The thickness of the boom plate determines the length of the matrix
[7], [8]
.
Harm to the boom structure can bear upon nail growth, shape, size and, consequently, predispose the nail to infection. OM tin can invade whatever office of the smash just typically enters the boom's costless edge, sulci or damaged cuticles (run into Effigy two).
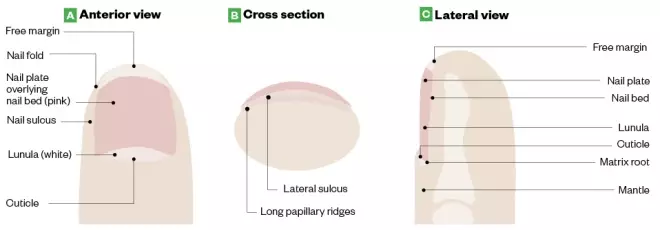
Figure 2: Anatomy of a salubrious toenail
Source: LeBlond RF, Brown DD, Suneja M & Szot JF. DeGowin's Diagnostic Exam, tenth ed. McGraw-Loma
Onychomycosis can invade any part of the nail simply typically enters the nail's complimentary edge, sulci or damaged cuticles.
Where OM infects the area underneath the nail plate, the infection produces a thick hyperkeratotic nodule that contains clusters of branching filaments (hyphae) called dermatophytoma (see Photoguide: A)[nine]
. Consequently, the nail becomes severely deformed and tin can cause boom lifting, brittleness and discoloration, which may result in acute pain[10]
. The abnormal thickness of the nail may pb to soft tissue breakdown and/or infection resulting in inflamed subcutaneous tissue (cellulitis), ulceration in the nail bed (subungual ulceration) and/or bone infection (osteomyelitis)[10]
.
Causes
Dermatophytes
Around 85–ninety% of OM cases are caused by dermatophytes (fungal organisms that require keratin for growth), such equally Trichophyton rubrum and Trichophyton
mentagrophtyes
[five], [11]
. Dermatophytes are highly resistant and tin survive for long periods of time, peculiarly in moist and dark environments[12], [xiii]
, which may explain why toenails are more than susceptible to OM than fingernails.
Non-dermatophyte moulds
Around 2–v% of cases of OM are caused by non-dermatophyte moulds, such equallyScopulariopsis,Scytalidium,Aspergillus,Fusarium andAcremonium species that typically affect toenails. Fingernails are rarely affected[5], [xi]
.
Yeasts
Candida spp. is responsible for 5–10% of OM infections, affecting fingernails more than often than toenails[14]
.

Photoguide: Types of onychomycosis
Source: Shutterstock.com / Courtesy of Marion Yau
Types of onychomycosis
Distal lateral subungual onychomycosis
The virtually common type of OM is distal lateral subungual onychomycosis (DLSO) (see Photoguide: B). It is characterised by build-upward of soft xanthous keratin between the boom plate and smash bed (subungual hyperkeratosis), detachment of the smash from the boom bed (onychosis) and skin infection around the nail (paronychia). DLSO spreads proximally to the boom matrix[15]
.
White superficial onychomycosis
Cases of white superficial onychomycosis (see Photoguide: C) are characterised by distinct white 'islands' on the blast surface, which gradually spread to the entire nail, causing it to get soft and crumbly[15]
.
Endonyx onychomycosis
White milky patches without subungual hyperkeratosis (build of keratin underneath the smash) indicate endonyx onychomycosis (EO) (see Photoguide: D). Pitting is involved with splitting of the nails. EO usually affects fingernails[fifteen]
.
Proximal subungual onychomycosis
Affecting fingernails and toenails, proximal subungual onychomycosis (PSO) (see Photoguide: E) is oft found in, simply not unique to, patients with HIV. The fungal infection begins at the cuticle and the smash fold earlier penetrating the nail plate. PSO is characterised by white discoloration that usually includes paronychia with some discharge[15]
.
Total dystrophic onychomycosis
The most avant-garde type of OM is full dystrophic onychomycosis (meet Photoguide: F), which invades the blast plate, boom bed and nail matrix causing astringent smash dystrophy. At that place can exist chronic swelling at the distal phalanx with the affected smash actualization thickened, xanthous-chocolate-brown in color and severely deformed[15]
.
Diagnosis
Despite OM having distinct clinical features, around half of nail dystrophy cases are caused by fungal infection and, therefore, clinical test lonely is rarely sufficient to diagnose OM[1]
.
Characteristics are shared with other smash diseases, such equally psoriasis, lichen planus or bacterial infections (see Tabular array 1). In improver to examining the nail(s) affected, pharmacists should enquire the patient the following questions to help plant a diagnosis[sixteen]
:
- How long have you lot had this condition?
- Do you lot take any skin disorders such every bit psoriasis, lichen planus, athlete's foot?
- Have you had the smash tested for mucus or any nail diseases?
- Have you suffered any trauma?
- Exercise you lot accept any family unit history of fungal nail infection?
- What is your occupation? (Jobs that involve the individual coming into contact with water may increase gamble of OM)
- Do your nails/toenails hurt?
- Does the issue bear upon daily activities such equally walking or standing?
Ideally, OM should exist confirmed past direct microscopy and cultures to eliminate non-infective differential diagnosis, to identify mixed infections and to discover resistant OM[5], [17]
. Effectually 30% of culture examinations are reported as imitation negative[eighteen]
and where OM is strongly suspected in the presence of a negative culture, the test should be repeated.
The British Association of Dermatologists (BAD) supports laboratory investigation prior to commencing oral treatment, which is in support of guidance from Public Health England (PHE)[5],[16]
. However, this guidance suggests that oral treatment can exist offered despite negative findings if at that place is a strong clinical suspicion[5],[x],[fifteen]
. Guidance for use of topical medications for DLSO is less clear and although investigations would nowadays good do, these treatments have minimal associated risks compared with oral handling. Still, incomplete sample drove could accept a major impact on faux negatives. Fourth dimension constraints and continuity in working patterns should exist considered as culture and microscopy results may take 2–half-dozen weeks to come back.
| Clinical indicators | Clarification |
|---|---|
| Punctate leukonychia | White spots on the nails; leukonychia is total whitening of the nail plate |
| Trauma or injury | Very similar advent of onychomycosis, causing the nail to lift from the smash bed (onycholysis), thicken (onychauxis) or develop white marker |
| Psoriasis | Pitting of the nails; yellow-red nail discolouration nether the blast plate that resembles a drop of blood or oil |
| Lichen planus | Ridged nails, melanonychia, thinning of the blast plate and smash dystrophy |
| Yellow nail syndrome | Loss of cuticle, yellow-light-green discolouration of the nails with thickening and curvature |
| Anaemia | Abnormal shape of the fingernail (koilonychia) with thinning, raised ridges and an inwards curve |
| Chronic eczema | Pitting of the nail with ridging, adjacent skin involvement with vesicles, scaling and erythema |
| Chronic renal failure | Proximal nail bed whiteness and distal nail bed red/pink/brown discolouration (called one-half and one-half nails); absent lunula and tiny blood clots under the nail (splinter haemorrhages) |
| Source: Neale'south Disorders of the Human foot[19] , Onychomycosis (Tinea unguium, Blast fungal infection)[twenty] | |
On examination, pharmacists should consider the following factors and patient groups and it may be necessary to refer the patient to a podiatrist or their GP:
- The infection affects more than two nails or more than half of the nail;
- At that place is nail dystrophy or destruction;
- The nail condition appears to be other than DSLO (differential diagnosis by pharmacists is essential to ensure the patient received the correct treatment — if there is any dubiousness of the diagnosis, the patient should be referred to a podiatrist or their GP);
- Patients with atmospheric condition that predispose them to fungal infections (eastward.k. immunosuppression, diabetes, peripheral circulatory disorders);
- Pregnant or breastfeeding women;
- Patients aged under 18 years;
- If there is no improvement after three months of treatment.
Treatment
The management of OM depends on the type, extent and severity of nail involvement, symptoms and pre-existing conditions. The aim of handling is to eradicate the pathogen, restore the smash and forestall re-infection. OM is challenging to treat and affected nails may never return to normal as the infection may accept caused permanent damage.
Equally OM has a high relapse rate of xl–70%[five]
, communication on preventative and appropriate cocky-care strategies to avoid re-infection should exist offered to patients.
Topical treatments
The compact and hard nature of the nail beefcake means topical drug penetration tin can be poor, with the concentration reducing by one,000 times from the outer to inner areas[v]
.
The BAD advises the employ of monotherapy topical antifungal agents to be restricted to:
- Superficial white onychomycosis (except for transverse or striate infections);
- Early on DLSO (except where longitudinal streaks be) without lunula involvement and where less than 80% of the nail plate is affected;
- When systemic antifungals are contraindicated.
Amorolfine
The but topical boom lacquer bachelor in the United kingdom for over-the-counter (OTC) purchase is amorolfine. It is licensed for mild (not more than than two nails afflicted) DLSO and patients aged 18 years or over. Amorolfine is a broad-spectrum constructed fungicidal with high action against dermatophytes, also as other fungi, yeasts and moulds. It is bachelor as a 5% lacquer that should be applied once or twice per calendar week[sixteen], [21]
. PHE recommend a treatment duration of 6 months for fingernails and 12 months for toenails, so adherence is essential[16]
.
Earlier application, patients should be brash to file downwardly the affected nail surfaces using a single-apply boom file, clean the nail surface with the supplied swab and dry out the nail surface[16]
. Patients should be reminded that this procedure should be repeated for sequential treatments; a footstep that is commonly missed out. Sterile cotton fiber buds should be used to apply the lacquer to avoid contagion.
Amorolfine maintains clinical efficacy in the blast for 14 days after treatment; however, twice-weekly application results in better outcomes compared with once-weekly awarding (71% versus 76% mycological cure)[22], [23]
. Compliance is essential; pharmacists should encourage patients to go along the handling, given the prolonged treatment elapsing of 6–12 months. Side effects are rare and express to nail disorders (e.1000. discolouration, and broken and brittle nails), which may be related to OM itself.
Tioconazole
The BAD recommends tioconazole, a prescription-only medicine (POM), for superficial and distal OM[5]
. Tioconazole is an imidazole derivative with a broad spectrum of activity against dermatophyte and yeast-like fungal species. Information technology is available as a 283mg/mL medicated nail lacquer and is applied to afflicted nails twice a 24-hour interval. Treatment duration ranges from vi–12 months depending on the pathogen, the severity and the location of the infection. Common side effects include mild and transient local irritation that usually presents during the first week of treatment[24]
.
Systemic therapy
For adults with confirmed OM, systemic therapy is brash when self-intendance strategies with or without topical therapy are unsuccessful or inappropriate. A recent Cochrane systematic review of oral antifungal treatments for toenail OM in more than ten,000 patients found loftier-quality bear witness indicating that terbinafine and azoles were effective treatments for mycological and clinical cure compared with placebo[11]
.
Terbinafine and itraconazole are considered the mainstay of oral therapy for OM, although terbinafine is by and large preferred over itraconazole attributable to ameliorate cure rates compared with azole in toenail OM[xi],[16]
. Other systemic therapies are available (see Table 2).
| Treatment | Contraindication and cautions | Dosing | Monitoring | Common adverse reactions |
|---|---|---|---|---|
| Terbinafine (first or second line) | Risk of developing lupus erythematosus-like effect; worsens symptoms of psoriasis | 250mg/day for vi weeks (fingernails) or 3–12 months (toenails) | Liver function: 4–half dozen weeks | Abdominal discomfort, anorexia, arthralgia, diarrhoea, dyspepsia, headache, myalgia, nausea, rash, urticaria[25] |
| Itraconazole (first or second line) | Risk of heart failure; avoid giving to patients with ventricular dysfunction or centre failure | 200mg once daily for 3 months, then 200mg twice daily for 7 days, repeated at 21 days. Fingers require ii courses, toes crave iii courses and persistent infections require an additional course of treatment | Liver function: four–half-dozen weeks | Abdominal pain, diarrhoea, dyspnoea, headache, hepatitis, hypokalaemia, nausea, rash, taste disturbances, vomiting[26], [27] |
| Fluconazole (tertiary line) | Currently non licensed for use in onychomycosis | Fingernails: 150–450mg one time per week for 3 months; toenails: 150–450mg once per calendar week for half dozen months | — | Abdominal discomfort, diarrhoea, flatulence, headache, nausea, rash[28] |
| Griseofulvin (4th line) | — | Fingernails: 500–1,000mg daily for 6-9 months; toenails: 500–1,000mg daily for 12–eighteen months | — | Abdominal pain, agitation, confusion, depression, diarrhoea, dizziness, dyspepsia, fatigue, glossitis, hepatotoxicity, impaired hearing, kidney failure, leucopenia, menstrual disturbances, nausea, peripheral neuropathy, photosensitivity, rash, slumber disturbances, systemic lupus erythematosus, taste disturbances, vomiting[29] |
| Ameen K, Lear JT, Madan Fiveet al. British Clan of Dermatologists' guidelines for the direction of onychomycosis 2014.Br J Dermatol 2014;171(5):937–958[5] | ||||
Combination therapy
Topical and systematic combination therapy may provide synergistic antimicrobial activity. The BAD recommends this for patients who have responded poorly to topical treatment alone[5]
. Amorolfine five% boom lacquer with systemic antifungals has been supported by a meta-analysis and systematic review to provide a college percentage of full OM clearance compared with monotherapy of systemic terbinafine, without an increase in adverse effects[30]
.
Photodynamic therapy
Photodynamic therapy combines low-cal irradiation and a photosensitising drug to crusade destruction of selected cells. Laser therapies, such as neodymiumyttrium-aluminum-garnet and depression-level laser, are aimed to selectively inhibit fungal growth[31]
. These alternative therapies may be appropriate because they are selective to local infection and avert systemic side effects; however, robust data are scarce[5]
and they are not offered on the NHS.
Lifestyle communication
Co-ordinate to the National Institute for Wellness and Care Excellence (Squeamish), patients require advice effectually foot intendance in guild to avoid and minimise exposure to situations that predispose individuals to OM (eastward.g. prolonged exposure to damp conditions, occlusive footwear, prevention of damaged nails and to ensure meticulous hygiene of the affected foot)[xiv]
.
Treatment must include a combination of proper hygiene and foot care as the risk of reinfection is high. Cocky-care to prevent infection should be stringently proficient until the fungus is eradicated, which may take up to 18 months[xiv]
.
Pharmacists should advise patients on nail care, washing and drying feet daily, using the correct footwear and encouraging the use of antifungal powder to assist keep shoes pathogen free. See Box for important self-care messages.
Box: Lifestyle advice for human foot care and hygiene
Do:
- Maintain practiced foot hygiene by washing anxiety daily, drying properly (especially in between the toes);
- Minimise exposure to environments that amass onychomycosis (eastward.g. warm, damp atmospheric condition);
- Wearable well-fitted shoes that are non-occlusive to prevent trauma and limit perspiration;
- Replace all onetime shoes and quondam socks to prevent re-infection[32]
; - Wear breathable or antimicrobial socks (e.g. cotton, bamboo or sliver fibre);
- Treat all family members to prevent cantankerous infection;
- Avoid nail trauma.
Do non:
- Use cosmetic nail varnishes or artificial nails;
- Share blast clippers with others;
- Walk without footwear in public areas (eastward.g. gym, hotel rooms, saunas);
- Cut nails also brusque.
When to refer to podiatry
Before initiating topical or oral therapy, patients should ideally exist referred to a podiatrist for nail trimming and debridement. This assists with removing as much fungus as possible and improves topical drug penetration. Debridement alone cannot exist recommended for the treatment of OM; patients using a combination of debridement and topical boom lacquer have shown a meaning comeback in mycological cure compared with debridement only[23]
. Patients with nail trauma owing to footwear, dystrophic toenails affecting other toes or who depict discomfort when walking owing to thickened toenails should also be referred.
When there is handling failure with topical, oral and combination therapies, a podiatrist may be able to bear out a chemic or surgical nail avulsion (total nail removal or partial avulsion).
If there is uncertainty over the original diagnosis, or where no comeback has been seen with treatment, pharmacists should refer patients to a podiatrist or their GP.
Supported past RB
RB provided fiscal support in the production of this content.
The authors were paid by The Pharmaceutical Journal to write this article and full editorial control was maintained by the journal at all times.
References
[1] Elewski BE. Onychomycosis: pathogenesis, diagnosis, and direction. Clin Microbiol Rev 1998;11(3):415–429. PMID: PMC88888
[2] Gupta AK, Versteeg SG & Shear NH. Onychomycosis in the 21st century: an update on diagnosis, epidemiology, and handling. J Cutan Med Surg 2017;21(6):525–539. doi: 10.1177/1203475417716362
[3] Sigurgeirsson B & Baran R. The prevalence of onychomycosis in the global population: a literature study. J Eur Acad Dermatol Venereol 2014;28(eleven):1480–1491. doi: 10.1111/jdv.12323
[4] Eichenfield LF & Friedlander SF. Pediatric onychomycosis: the emerging part of topical therapy. J Drugs Dermatol 2017;16(2):105–109. PMID: 28300851
[5] Ameen M, Lear JT, Madan V et al. British Association of Dermatologists' guidelines for the management of onychomycosis 2014. Br J Dermatol 2014;171(5):937–958. doi: 10.1111/bjd.13358
[6] Frowen P, O'Donnell 1000 & Burrow JG. In: Lorimer D (ed). Podiatric management of the elderly. Neale'due south Disorders of the Foot. 8th ed. Churchill Livingstone; 2010.
[vii] Ross MH & Pawlina W. Histology: A text and atlas. fourth edition. Lippincott Williams & Wilkins; 2006. p447.
[8] Haneke E. Anatomy of the boom unit and the nail biopsy. Semin Cutan Med Surg 2015;34(two):95–100. doi: 10.12788/j.sder.2015.0143
[9] Campos South & Lencastre A. Dermatoscopic correlates of nail appliance affliction. In: Imaging in dermatology. Elsevier. 2016;43–58.
[10] Rubin AI, Jellinek NJ, Daniel RC, Scher RK (eds). Scher and Daniel'south nails: Diagnosis, surgery, therapy. 4th ed. Springer; 2018.
[11] Kreijkamp-Kaspers S, Hawke Grand, Guo L et al. Oral antifungal medication for toenail onychomycosis. Cochrane Database Syst Rev 2017;(7):CD010031. doi: 10.1002/14651858.CD010031.pub2
[12] Abd Elmegeed ASM, Ouf SA, Moussa TAA & Eltahlawi SMR. Dermatophytes and other associated fungi in patients attending to some hospitals in Egypt. Braz J Microbiol 2015;46(3):799–805. doi: 10.1590/S1517-838246320140615
[xiii] White TC, Findley Thousand, Dawson TL Jr et al. Fungi on the skin: dermatophytes and Malassezia. Common cold Bound Harb Perspect Med 2014;4(viii): a019802. doi: 10.1101/cshperspect.a019802
[xiv] National Constitute for Wellness and Care Excellence. Fungal nail infection; 2014. Available at: https://cks.dainty.org.united kingdom of great britain and northern ireland/fungal-blast-infection#!diagnosissub:i (accessed Nov 2018).
[15] Singal A & Khanna D. Onychomycosis: Diagnosis and management. Indian J Dermatol Venereol Leprol 2013;77(6):659–672. doi: 10.4103/0378-6323.86475
[sixteen] Public Health England. Fungal skin and nail infections: Diagnosis and laboratory investigation. Public Health England: Protecting and improving the nation'southward health 2017. Available at: https://avails.publishing.service.gov.united kingdom of great britain and northern ireland/regime/uploads/system/uploads/attachment_data/file/619770/Fungal_skin_and_nail_infections_guidance.pdf (accessed Nov 2018)
[17] Fletcher CL, Hay RJ & Smeeton NC. Onychomycosis: the development of a clinical diagnostic aid for toenail affliction. Part I. Establishing discriminating historical and clinical features. Br J Dermatol 2004;150(4):701–705. doi: ten.1111/j.0007-0963.2004.05871.10
[xviii] Eisman S & Sinclair R. Clinical Review. Fungal blast infection: diagnosis and management. BMJ 2014;(348):g1800. doi: x.1136/bmj.g1800
[nineteen] Frowen P, O'Donnell M & Burrow JG. In: Lorimer D (ed). The pare and nails in podiatry. Neale's Disorders of the Pes. 8th ed. Churchill Livingstone; 2010.
[20] Lipner, SR, Scher, RK & Ashourian, N. Onychomycosis (Tinea unguium, Nail fungal infection); 2017. Available at: https://www.dermatologyadvisor.com/dermatology/onychomycosis-tinea-unguium-nail-fungal-infection/commodity/691367/ (accessed November 2018)
[21] Electronic Medicines Compendium: Aspire Pharma Ltd. Amorolfine 5% w/v Medicated Nail Lacquer; 2018. Available at: https://www.medicines.org.great britain/emc/product/7414/smpc (accessed November 2018)
[22] Reinel D. Topical treatment of onychomycosis with amorolfine 5% nail lacquer: comparative efficacy and tolerability of once and twice weekly use. Dermatology 1992;184(1):21–24. doi: 10.1159/000247612
[23] Malay DS, Yi S, Borowsky P et al. Efficacy of debridement lonely versus debridement combined with topical antifungal nail lacquer for the handling of pedal onychomycosis: a randomized, controlled trial. J Foot Ankle Surg 2009;48(3):294–308. doi: 10.1053/j.jfas.2008.12.012
[24] Electronic Medicines Compendium: Creo Pharma Limited. Tioconazole 283 mg/ml medicated nail laquer; 2017. Available at: https://www.medicines.org.great britain/emc/production/8643/smpc (accessed November 2018)
[25] British National Formulary. Terbinafine; 2018. Available at: https://world wide web.medicinescomplete.com/#/content/bnf/_203423860 (accessed November 2018)
[26] Electronic Medicines Compendium: Sandoz Limited. Itraconazole 100mg capsules; 2018. https://world wide web.medicines.org.uk/emc/product/7297/smpc (accessed November 2018)
[27] British National Formulary. Itraconazole; 2018. https://world wide web.medicinescomplete.com/#/content/bnf/_398441057 (accessed Nov 2018)
[28] British National Formulary. Fluconazole; 2018. https://world wide web.medicinescomplete.com/#/content/bnf/_870309169?hspl=Fluconazole (accessed November 2018)
[29] British National Formulary. Griseofulvin; 2018. https://www.medicinescomplete.com/#/content/bnf/_101711937 (accessed Nov 2018)
[30] Feng X, Xiong X & Ran Y. Efficacy and tolerability of amorolfine five% nail lacquer in combination with systemic antifungal agents for onychomycosis: A meta-analysis and systematic review. Dermatologic Therapy 2017;thirty(three). doi: 10.1111/dth.12457
[31] Kolodchenko VY & Baetul Half dozen. A novel method for the treatment of fungal nail illness with 1064 nm Nd:YAG. J Light amplification by stimulated emission of radiation Health Acad; 2013. Available at: https://world wide web.laserandhealthacademy.com/media/objave/academy/priponke/42_47___kolodchenko___onychomycosis___jlaha_2013_1.pdf (accessed Nov 2018)
[32] Broughton RH. Reinfection from socks and shoes in tinae pedis. Br J Dermatol 1955;67(7):249–254. PMID:13239972
Last updated
Source: https://pharmaceutical-journal.com/article/ld/how-to-treat-fungal-nail-effectively
Posted by: dickensevervall.blogspot.com


0 Response to "How Long To Heal A Nail Fungis W Lamisil Oral"
Post a Comment